What Are Weeping Legs? +7 Tips How to Manage Them
Discover 7 effective tips for managing weeping legs naturally. Learn practical strategies for skin care, circulation, and daily comfort.


Have you ever experienced the uncomfortable sensation of fluid seeping through your skin, leaving your legs damp and irritated? Weeping legs can turn simple daily activities into challenging ordeals, affecting both comfort and confidence. This condition occurs when excess fluid escapes through the skin due to fluid retention and imbalances in circulation.
While weeping legs may appear concerning, there’s good news – with proper management strategies, you can maintain skin integrity and improve comfort. In this guide, we’ll explore the causes, symptoms, and seven effective tips for managing weeping legs.
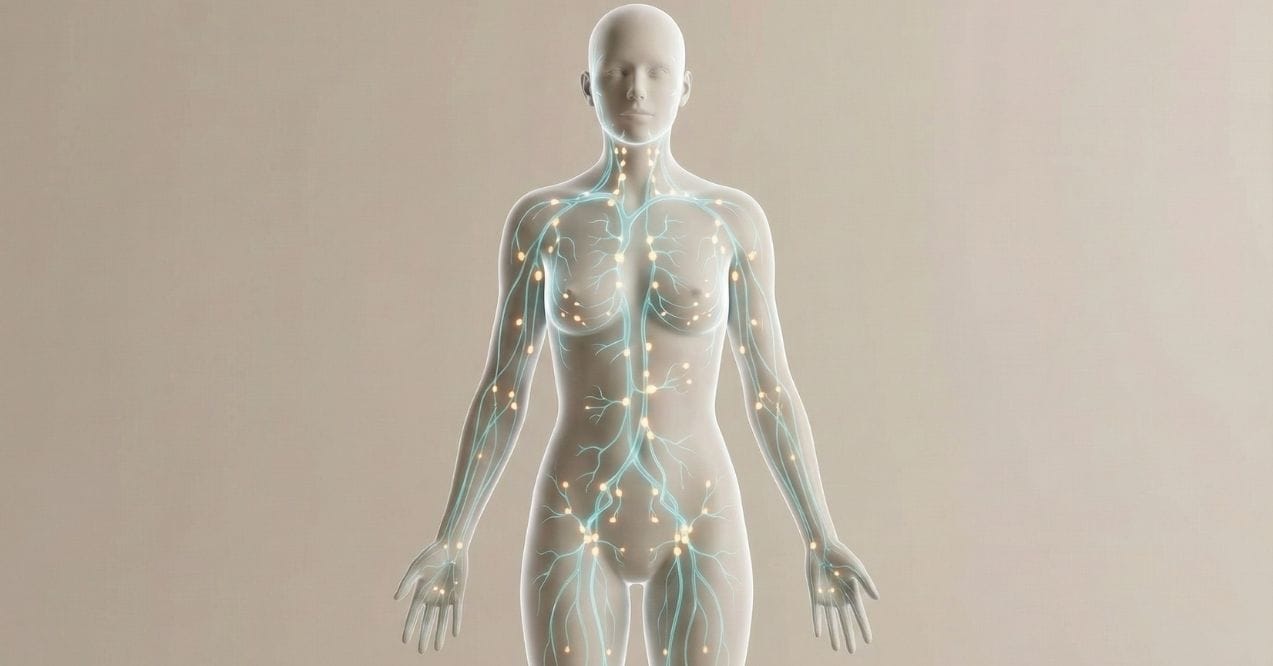
What Are Weeping Legs?

Weeping legs happen when your body keeps too much fluid. This extra fluid builds up and starts to leak out of your skin. It’s like a sponge that’s too full and starts to drip. Weeping legs usually happen with swelling, poor blood flow, and weak skin.
Important: Weeping legs aren’t a disease. They are a sign that your body is having trouble managing fluid. It’s key to figure out why this is happening to keep your skin healthy and comfy.
Main Causes of Weeping Legs
Understanding why fluid seeps from legs involves considering multiple factors. Weeping legs often occur when several issues combine and overwhelm the body’s fluid management.
- Fluid retention – When the body holds onto extra fluid, it builds pressure in tissues. This pressure seeks an escape route, often through the skin, especially in vulnerable areas. High sodium intake and insufficient water intake can contribute to fluid retention.
- Poor circulation – Healthy blood flow helps transport fluid throughout the body. If circulation is slow, especially in the legs, fluid can accumulate instead of returning properly, creating pressure that forces fluid through weakened skin.
- Skin barrier vulnerability – The skin acts as a protective barrier. With age or certain conditions, this barrier can weaken. Fragile skin cannot hold built-up fluids, allowing them to seep through small openings.
- External factors – Environmental conditions can worsen weeping legs. Heat can increase swelling, while humidity affects how quickly moisture evaporates from the skin. Certain fabrics or prolonged sitting or standing can also aggravate fluid accumulation.
- Lifestyle contributions – Daily habits impact fluid balance. Limited movement, long periods in one position, and certain diets can increase fluid retention and seepage through vulnerable skin.
Seven Tips for Managing Weeping Legs
Managing weeping legs requires a comprehensive approach that addresses multiple aspects of skin health and circulation. Understanding how to stop fluid leaking from legs involves targeted strategies that work together to support your body’s natural processes. These practical solutions can help you maintain comfort and skin integrity.
1. Maintain Clean and Dry Skin
Keeping affected areas clean and dry creates an environment where healing can occur and prevents additional complications. This fundamental step helps protect vulnerable skin from further damage.
- Use lukewarm water (not hot) with mild, fragrance-free cleansers that won’t strip natural oils
- Pat skin gently with a soft towel rather than rubbing, which can damage fragile skin
- Allow skin to air dry completely before applying any products or dressings
- Consider zinc-based barrier creams or ointments that create a protective moisture-resistant shield
- Change any damp clothing or bedding promptly to maintain a dry environment
2. Use Compression Garments

Compression garments provide gentle, consistent pressure that helps manage fluid movement within tissues and supports proper circulation back toward the heart.
- Select properly fitted compression stockings or wraps based on your specific needs
- Apply compression in the morning before fluid accumulates throughout the day
- Ensure even pressure without creating tight spots that could restrict circulation
- Remove compression periodically to check skin condition and allow for cleaning
- Consider graduated compression garments that provide more pressure at the ankle and less up the leg
Remember that proper fit is crucial – compression should feel supportive but never painful or overly restrictive.
3. Try Supplements
Certain nutrients can support skin health and help maintain proper fluid balance throughout the body.
- Omega-3 fatty acids may help maintain skin integrity and support healthy inflammation response
- Vitamin C contributes to collagen production, which provides structure to skin
- Magnesium plays a role in maintaining cellular fluid balance
- Antioxidants help protect skin cells from damage
- B-complex vitamins support overall tissue health
If you’re exploring the best vitamins for tired legs or considering lymph system supplements, always consult with a healthcare professional before starting any new supplement regimen, especially if you have existing health conditions or take other supplements.
4. Elevate Legs

Strategic elevation works with gravity to facilitate natural fluid drainage and reduce pressure within the tissues of your legs.
- Raise legs above heart level when resting to encourage fluid movement
- Use several pillows under your legs while lying down
- Try specialized leg elevation pillows designed for comfortable positioning
- Install a footrest under your desk or use an ottoman when sitting
- Elevate for 20-30 minutes several times daily for best results
This simple practice can significantly reduce swelling and help manage fluid accumulation throughout the day.
5. Hydrate Skin
Well-moisturized skin maintains its natural barrier function better than dry skin, helping to prevent microscopic breaks where fluid can escape.
- Apply emollient-rich moisturizers immediately after bathing while skin is still slightly damp
- Look for products with ceramides, which help maintain the skin’s protective barrier
- Choose fragrance-free formulations to minimize irritation potential
- Apply moisturizers in a thin, even layer, avoiding excess that could create a damp environment
- For very dry skin, consider products containing urea or lactic acid which help maintain natural moisture
Properly hydrated skin is more resilient against the stresses that contribute to fluid seepage.
6. Incorporate Exercises
Movement stimulates circulation and helps your body naturally process and eliminate excess fluid.
- Try seated ankle circles: rotate your feet 10 times in each direction
- Practice gentle leg lifts while sitting or lying down
- Perform calf pumps by raising and lowering your heels while seated
- Consider water exercises which provide natural compression
- Take short, frequent walks throughout the day
Even small amounts of movement can make a significant difference when done consistently throughout the day.
7. Limit Unhealthy Foods

Your dietary choices directly impact fluid retention and skin health. Strategic adjustments can help manage fluid balance from the inside out.
- Reduce sodium intake by limiting processed foods and added salt
- Increase consumption of potassium-rich fruits and vegetables to help balance fluid levels
- Choose foods high in natural antioxidants like berries and leafy greens
- Stay well-hydrated with water to support proper fluid movement
- Consider incorporating herbs for lymphatic system
- Limit alcohol and caffeine, which can contribute to dehydration
When to Seek Professional Guidance
While many cases of weeping legs can be managed with home care strategies, certain situations warrant professional attention. Be alert to these key indicators that suggest it’s time for a professional assessment:
- Persistent fluid leakage that doesn’t improve after 1-2 weeks of consistent home care
- Increasing redness, warmth, or tenderness around the affected area
- Sudden or significant increase in swelling that doesn’t respond to elevation
- Development of skin changes such as discoloration or texture changes
- Unusual odor from the weeping fluid
- Increasing pain or discomfort that interferes with daily activities
- Changes in temperature, such as the area feeling unusually warm
- Formation of open areas in the skin that don’t show signs of improvement
Remember that early intervention often leads to better outcomes. If you’re unsure whether your symptoms warrant professional attention, it’s generally better to err on the side of caution and seek an evaluation.
Conclusion
Managing weeping legs successfully requires a multi-faceted approach combining proper skin care, strategic movement, appropriate compression, and mindful dietary choices. By implementing these seven practical strategies consistently, you can take meaningful steps toward reducing discomfort and supporting skin integrity.
Remember that persistence with these methods often yields the best results. Pay attention to how your body responds and adjust your approach as needed. While these tips provide a solid foundation, everyone’s situation is unique. Don’t hesitate to seek professional guidance if symptoms persist despite your efforts.
With proactive management, you can maintain skin health, enhance comfort, and improve your daily quality of life.
Fluid seeping from legs can indicate an underlying issue that needs attention. While not always an emergency, persistent leaking should be addressed promptly to maintain skin health and prevent potential complications with tissue integrity.
Weeping skin on legs typically results from excess fluid buildup, compromised circulation, fragile skin barriers, and environmental factors. The combination of these issues overwhelms the body’s natural drainage systems, forcing fluid through vulnerable skin areas.
Manage weeping sores by keeping the area clean and dry, applying appropriate moisture barriers, using compression garments, elevating legs regularly, and supporting skin health with proper hydration and nutrition. Consistent care helps maintain skin integrity.
Gentle walking can benefit weeping legs by promoting circulation and helping fluid move through proper channels. Start with short, comfortable walks and gradually increase duration as tolerated. Movement supports the body’s natural drainage systems.
Sign up for our Healthy Living newsletter!
Advertisement. This site offers health, wellness, fitness and nutritional information and is designed for educational purposes only. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk.