6 Stages of Varicose Veins: Identifying Symptoms at Each Level
Discover the 6 stages of varicose veins, from early spider veins to serious ulceration. Learn to identify symptoms and when to seek help.


Varicose veins affect approximately 23% of adults worldwide, appearing as swollen, twisted blood vessels visible beneath the skin’s surface. These vascular changes develop gradually through distinct stages of varicose veins, each with recognizable symptoms that signal progression.
While common in the legs, these vascular alterations can affect various body areas and may cause discomfort, heaviness, or aesthetic concerns. Recognizing early indicators allows for timely intervention, potentially alleviating symptoms and supporting vascular health.
Understanding Varicose Veins
Varicose veins develop when the one-way valves within your veins weaken or become damaged. These valves normally ensure blood flows efficiently toward your heart, preventing backward movement. When compromised, blood pools in the veins, causing them to stretch, twist, and enlarge beneath the skin surface.
Several factors contribute to the development of varicose veins:
- Genetic predisposition – For those wondering are spider veins genetic, those with family members affected by vascular irregularities could face a higher risk
- Age-related changes – Vein walls naturally lose elasticity over time
- Prolonged positions – Standing or sitting for extended periods restricts proper circulation
- Hormonal fluctuations – Particularly during pregnancy, these may increase pressure on leg veins
- Weight factors – Extra weight places additional pressure on veins
- Sedentary lifestyle – Reduces muscle contractions needed to assist blood flow upward against gravity
Stage 1 – Spider Veins (Telangiectasia)

The journey through the stages of varicose veins typically begins with spider veins, medically known as telangiectasia. These small, thin vessels appear close to the skin’s surface, creating a web-like pattern that resembles tree branches or spider webs. Their appearance ranges from red to blue to purple, standing out visibly against the surrounding skin.
Early signs and symptoms of varicose veins at this stage are primarily cosmetic, with most individuals experiencing no physical discomfort. The affected areas may include:
- Outer thighs and calves
- Ankles
- Face (especially around the nose)
- Back of knees
While spider veins rarely cause physical symptoms, some people report mild itching or burning sensations around the visible veins. Though generally harmless, these small vessels represent the first indication of potential vascular changes occurring beneath the surface.
Stage 2 – Enlarged Varicose Veins
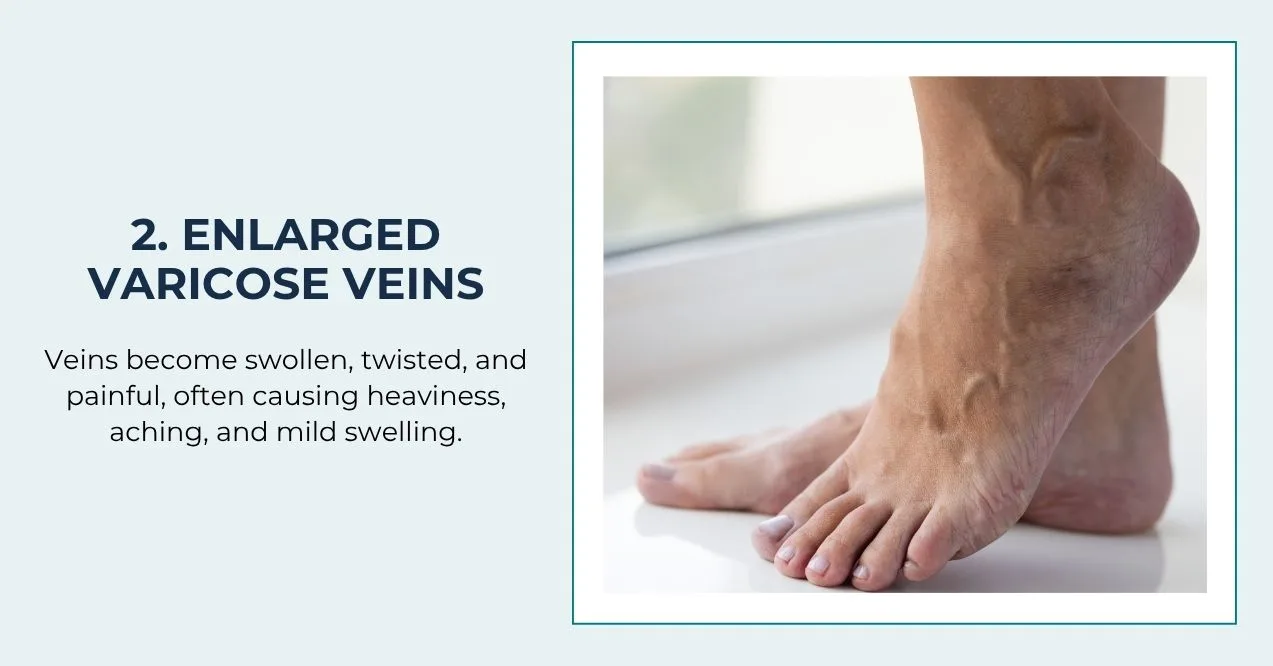
As the condition progresses beyond spider veins, the second of the varicose veins stages presents with more visible and physically noticeable symptoms. At this stage, veins become enlarged, twisted, and prominently bulge beneath the skin surface, typically appearing blue or dark purple in color.
Unlike the primarily cosmetic concerns of stage 1, individuals experiencing stage 2 often report physical discomfort:
- A persistent feeling of heaviness in the legs, especially after long periods of standing
- Aching or throbbing sensations that worsen throughout the day
- Muscle cramping, particularly at night
- Itching around the affected veins
- Mild swelling in the ankles and feet by evening
These enlarged vessels commonly appear on the legs, particularly on the backs of calves or along the inside of thighs. The veins may feel rope-like when touched and can protrude noticeably when standing or after prolonged sitting.
At this stage, symptoms typically intensify during warm weather or after extended periods without movement. Many people find temporary relief by elevating their legs or wearing compression garments that support proper circulation.
Stage 3 – Edema (Swelling)

The third stage in the progression introduces a significant new symptom: edema. This persistent swelling occurs primarily in the ankles and lower legs as the vascular irregularities begin to affect fluid balance in the surrounding tissues.
At this stage, blood pooling creates increased pressure within the veins, forcing fluid to leak into surrounding tissues. This fluid accumulation manifests as:
- Visible puffiness around the ankles that may extend upward to the calves
- A feeling of heaviness or fullness in the affected limbs
- Skin that appears shiny or stretched over swollen areas
- Indentations that remain after pressing on the swollen area (pitting edema)
- Discomfort that worsens throughout the day, particularly after standing or sitting
The swelling typically becomes more pronounced as the day progresses and may temporarily improve with nighttime rest and leg elevation. Many individuals notice their shoes feeling tighter by evening or sock marks leaving deeper impressions on their skin.
This stage signals that the vascular system is struggling to maintain proper fluid balance. The edema often fluctuates in severity, sometimes improving with lifestyle adjustments like regular movement, leg elevation, and compression garments. However, without appropriate attention, this stage may progress toward more concerning skin and tissue changes.
Stage 4 – Skin Changes

By the fourth stage, prolonged venous insufficiency begins to visibly alter the skin surrounding affected veins. These changes occur as tissues experience extended periods of poor circulation, resulting in limited oxygen and nutrient delivery to skin cells.
The skin undergoes several noticeable transformations:
- Brownish or reddish discoloration around the ankles and lower legs
- Thickening and hardening of skin texture, resembling leather
- Excessive dryness that may not respond to typical moisturizers
- Persistent itching that can become quite intense
- Increased sensitivity to touch or pressure
- Atrophic changes where skin becomes thin and fragile
- A shiny, taut appearance over affected areas
These skin changes typically begin near the ankles and may gradually extend upward. The discoloration occurs as hemosiderin, a breakdown product of red blood cells, deposits in the skin tissues. This staining often persists even with improved circulation.
The skin’s protective barrier function becomes compromised at this stage, making it more vulnerable to minor injuries and slower to heal from everyday scrapes or bumps. Some individuals also notice that hair growth diminishes in affected areas.
Without addressing the underlying vascular issues, these skin changes indicate advancing vascular insufficiency that may eventually lead to more serious tissue complications in subsequent stages.
Stage 5 – Healed Ulcers

The fifth stage represents a significant milestone in vascular progression, marked by the presence of healed ulcers. These smooth, often whitish scars indicate areas where the skin previously broke down completely but has since repaired itself.
Healed ulcers typically appear as:
- Irregular, slightly depressed areas of skin
- Tissue with distinctly different texture and color compared to surrounding skin
- Areas that may feel smoother and tighter than normal skin
- Patches that often have whitish centers surrounded by darker pigmentation
- Regions that may be more sensitive or less sensitive than surrounding tissue
These healed areas serve as important warning signs. Their presence indicates that circulation has deteriorated to the point where tissue breakdown has already occurred once, creating vulnerability for future breakdown.
Even though these ulcers have healed, the underlying vascular insufficiency often remains unresolved. Without proper attention to circulation support, these same areas face high risk of reopening, potentially developing into new, active ulcers.
Individuals at this stage should pay particular attention to protecting previously ulcerated areas from pressure, friction, and minor injuries. Careful skin monitoring, consistent use of compression garments, and regular movement to promote circulation become especially crucial to prevent regression to active ulceration and maintain the integrity of healed tissue.
Stage 6 – Active Ulcers

The sixth and most severe stage of vascular progression features active ulcers – open wounds that resist healing due to severely compromised circulation. This advanced stage represents the culmination of chronic venous insufficiency, where the skin and underlying tissues break down completely.
For those wondering what do varicose veins feel like at this advanced stage, the discomfort extends well beyond the earlier sensations of heaviness or aching:
- Open, persistent wounds typically located near the ankles or lower leg
- Moderate to severe pain that may interfere with daily activities and sleep
- Red, inflamed tissue surrounding the wound edges
- Clear, yellow, or blood-tinged drainage from the wound
- Unpleasant odor if bacterial colonization occurs
- Extreme sensitivity to even slight pressure or touch
- Difficulty walking or bearing weight on the affected limb
These ulcers develop when skin cells receive inadequate oxygen and nutrients for an extended period, eventually causing tissue death. The compromised immune response in these areas makes them particularly vulnerable to bacterial infections, which can further complicate healing.
Active ulcers require comprehensive care and should never be self-managed. They demand professional attention to address both the wound itself and the underlying vascular issues causing it. Without proper intervention, these wounds may persist for months or years, progressively enlarging and increasing the risk of serious complications.
When to Seek Medical Advice
Recognizing when to seek professional support for vascular concerns can prevent progression to more advanced stages. While early stages may respond well to self-care measures, certain symptoms warrant prompt medical attention.
Consider consulting a healthcare professional if you experience:
- Persistent leg pain that doesn’t improve with rest or elevation
- Swelling that doesn’t subside overnight or after leg elevation
- Skin changes including discoloration, hardening, or increased sensitivity
- Visible veins that become increasingly prominent or painful
- Itching or burning sensations that interfere with daily activities or sleep
- Any open sores or wounds on the legs that don’t heal within a few weeks
- Sudden, severe leg pain accompanied by swelling
Treatment Options for Varicose Veins
Managing vascular concerns involves a spectrum of approaches tailored to the stage and severity of the condition. From conservative measures to advanced interventions, several options can help alleviate symptoms and prevent progression.
Lifestyle modifications serve as foundation support for all stages:
- Regular walking and exercise to activate calf muscles
- Elevating legs above heart level when resting
- Avoiding prolonged standing or sitting
- Maintaining healthy weight to reduce pressure on veins
Compression therapy offers external support through specially designed stockings that improve circulation and reduce swelling.
For more visible or symptomatic veins, minimally invasive procedures include:
- Sclerotherapy – injection of solution that causes veins to collapse and fade
- Laser treatments – using light energy to close smaller veins
- Radiofrequency closure – using heat to seal affected vessels
Advanced stages may benefit from procedural interventions:
- Ambulatory phlebectomy – removal of larger veins through tiny incisions
- Endovenous techniques – using catheter-based systems to close problematic veins
The optimal approach depends on your specific symptoms, vein characteristics, and overall health status. Many treatments can be performed in outpatient settings with minimal downtime.
Supporting Vein Health Naturally
Beyond medical interventions, nutritional support can play a complementary role in promoting vascular wellness. For those seeking how to improve circulation in feet and legs through natural means, targeted supplements may offer additional support alongside lifestyle changes.
VenEase contains botanicals specifically selected to support vein health and proper circulation. This formula combines several research-backed ingredients:
- Rutin – A plant-based compound that supports lymphatic drainage, potentially reducing fluid retention and swelling while improving overall leg comfort
- Micronized Purified Flavonoid Fraction (MPFF) – Helps alleviate leg discomforts including heaviness and cramping while supporting the structural integrity of vein walls
- Horse Chestnut Extract – Shown to reduce leg discomfort and may offer support comparable to external compression methods by promoting vascular tone
- Butcher’s Broom – Contains natural compounds that support healthy vascular constriction and may help reduce fluid retention in the lower extremities

These botanical ingredients work synergistically to support overall vascular function, potentially complementing other approaches to leg health. When combined with regular movement, proper hydration, and leg elevation, these natural compounds may help maintain comfort and appearance of legs affected by vascular concerns.
Key Takeaways
Varicose veins progress through six identifiable stages, each with distinct symptoms ranging from minor spider veins to serious tissue complications. Recognizing these progression markers allows for timely intervention before advanced stages develop.
A spectrum of treatment options exists for every stage, from simple lifestyle modifications to specialized procedures that address specific vascular concerns. Many effective treatments now offer minimal recovery time and excellent outcomes when applied at appropriate stages.
For comprehensive support, consider incorporating natural supplements like Venease alongside medical approaches. These botanically-based formulations may complement other interventions by supporting vascular function from within, particularly when implemented early in the progression cycle.
While early-stage symptoms may temporarily improve with lifestyle adjustments, established varicose veins don’t typically disappear without intervention. The underlying vascular changes generally remain and may progress unless addressed through specific treatments that close or remove affected vessels.
No, varicose veins extend beyond cosmetic issues. They represent underlying vascular insufficiency that can progress to cause significant discomfort, swelling, skin changes, and in advanced stages, tissue breakdown leading to ulceration if left unaddressed.
Regular walking activates calf muscles that help pump blood upward. Elevate legs when resting, maintain healthy weight, avoid prolonged standing/sitting, stay hydrated, and consider compression garments during extended periods on your feet.
Consult with a healthcare provider before starting Venease, particularly if you have existing health conditions, take medications, are pregnant or nursing. Individual ingredients may interact with certain medications or may not be appropriate for specific health situations.
Sign up for our Healthy Living newsletter!
Advertisement. This site offers health, wellness, fitness and nutritional information and is designed for educational purposes only. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk.










