FODMAP Intolerance: What Is It? Symptoms and Solutions
Learn about FODMAP intolerance, its symptoms, triggers, and practical ways to manage it for better digestive health.


FODMAP intolerance can significantly impact digestion and overall comfort. For many, understanding this sensitivity is the first step to improving their well-being. FODMAPs are specific types of carbohydrates that some people find challenging to digest, leading to discomfort after meals. Recognizing the symptoms and identifying common triggers can help individuals make informed choices about their diet and lifestyle.
In this blog post, we’ll explore the essentials of FODMAP intolerance – what it is, its symptoms, how to identify triggers, and practical ways to support digestive health through dietary adjustments.
What is FODMAP Intolerance?
Wondering what is FODMAP intolerance? It happens when the body struggles to digest a specific group of carbohydrates called FODMAPs. These carbohydrates don’t absorb well in the small intestine. Instead, they pull water into the gut and ferment, producing gas as gut bacteria break them down. This process can cause bloating and other signs of digestive discomfort.
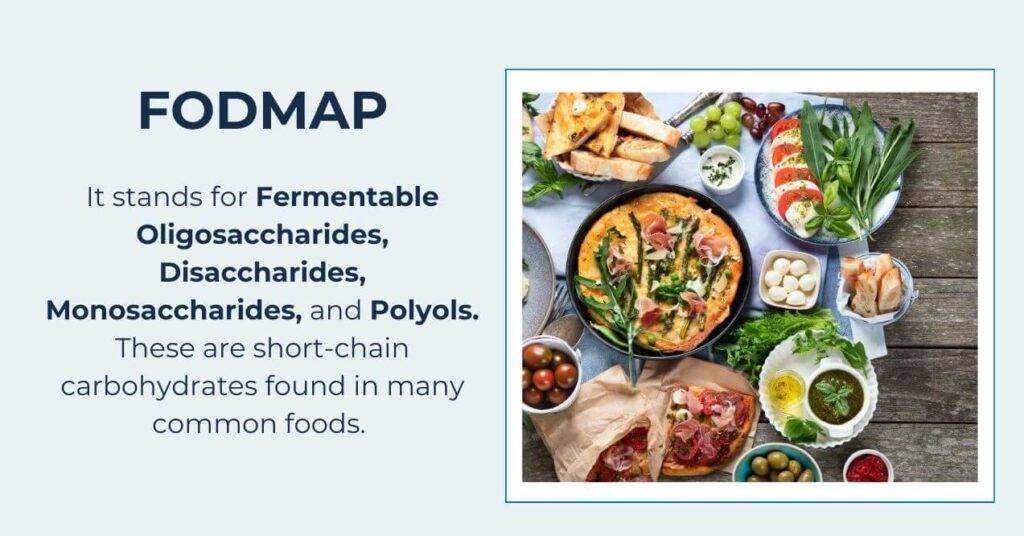
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates found in many common foods. Here’s a breakdown:
- Oligosaccharides – Found in wheat, onions, garlic, and legumes.
- Disaccharides – Lactose, found in milk and other dairy products.
- Monosaccharides – Fructose, found in fruits like apples and sweeteners like honey.
- Polyols – Sugar alcohols such as sorbitol and mannitol, found in some fruits, vegetables, and sugar-free products.
FODMAP intolerance differs from other food issues like allergies or sensitivities. It’s not about the immune system reacting to food but how these carbohydrates behave during digestion. Understanding this difference can help you identify and manage the triggers effectively.
Symptoms of FODMAP Intolerance
FODMAP intolerance occurs when certain carbohydrates ferment in the gut, triggering a range of uncomfortable digestive issues. These symptoms arise because FODMAPs pull water into the gut and produce gas as bacteria break them down. The result? Digestive discomfort like:
- Bloating
- Excess gas
- Noticeable changes in bowel habits.
FODMAPs vs. IBS

FODMAP intolerance symptoms can look like those of Irritable Bowel Syndrome (IBS), but the two are not the same. Both can cause bloating, abdominal discomfort, and irregular bowel movements. However, IBS is more complex, involving factors like stress and gut-brain interactions.
FODMAP intolerance is specifically tied to how the gut digests certain carbohydrates. For some people with IBS, managing FODMAP intake may help reduce symptoms. Still, not all IBS cases are linked to FODMAPs. Recognizing the difference can help you find the best way to manage your digestive health.
FODMAPs vs. Gluten Intolerance

Symptoms of FODMAP intolerance can overlap with those of gluten intolerance, but these are distinct conditions. Gluten intolerance, including celiac disease, involves an immune reaction to gluten – a protein found in wheat, barley, and rye – which can harm the small intestine.
In contrast, FODMAP intolerance relates to how the body digests certain carbohydrates. Wheat, for example, contains both gluten and FODMAPs, making it difficult to pinpoint the source of symptoms. Understanding whether your body reacts to gluten or FODMAPs is crucial for selecting the appropriate dietary approach.
Answering the Question: Is it FODMAPs?
FODMAP intolerance symptoms often emerge after eating high-FODMAP foods, but how do you know if FODMAPs are the problem? Start by asking yourself:
- Do symptoms like bloating or gas occur within hours of eating certain foods?
- Are high-FODMAP foods like garlic, onions, or dairy common triggers?
- Do symptoms improve when avoiding these foods?
If the answer is yes, FODMAPs may be involved. To confirm, consider a FODMAP intolerance test under the guidance of a healthcare professional. They can help rule out other conditions and pinpoint triggers using tools like food diaries or elimination diets. This process ensures you get tailored advice for managing symptoms and maintaining digestive comfort.
What Are FODMAP Intolerance Triggers?
Identifying FODMAP intolerance triggers often involves making dietary changes to understand which foods cause symptoms. By recognizing high-FODMAP foods and learning about their low-FODMAP substitutes, you can take steps to support digestive comfort.
High-FODMAP Foods
Certain foods are naturally high in FODMAPs and may cause symptoms in sensitive individuals. Common high-FODMAP foods include:
- Dairy – Milk, soft cheeses, yogurt, and ice cream.
- Fruits – Apples, pears, watermelon, and cherries.
- Vegetables – Garlic, onions, cauliflower, and asparagus.
- Grains – Wheat, rye, and barley.
- Sweeteners – High-fructose corn syrup, honey, sorbitol, and mannitol.
Low-FODMAP alternatives can help reduce symptoms. For example, replace milk with lactose-free milk, apples with bananas, and onions with onion-infused oil. These swaps allow you to enjoy a varied diet while avoiding discomfort.
The Low-FODMAP Diet
The low-FODMAP diet is a structured approach to identifying triggers. It has two key phases:
- Elimination Phase – This involves temporarily avoiding high-FODMAP foods. By reducing FODMAP intake, you can assess whether symptoms improve.
- Reintroduction Phase – Gradually add high-FODMAP foods back into your diet, one at a time. This helps pinpoint which foods trigger symptoms and which ones you can tolerate.
Remember, this process should ideally be done under the guidance of a healthcare professional to ensure a balanced diet and accurate results. Over time, it can provide a clear roadmap for managing FODMAP intolerance.
How to Manage FODMAP Intolerance?
Managing FODMAP intolerance requires a combination of dietary and lifestyle changes to minimize symptoms and support digestive health. Here’s how you can take control:
- Reduce high-FODMAP foods – Replace triggers with low-FODMAP alternatives, such as lactose-free dairy, gluten-free grains, and low-FODMAP fruits and vegetables.
- Read food labels – Check for hidden FODMAPs, such as high-fructose corn syrup or certain artificial sweeteners. Be cautious of packaged foods labeled “sugar-free,” as they often contain FODMAP-rich sugar alcohols like sorbitol or mannitol.
- Control portion sizes – Even low-FODMAP foods can cause discomfort if eaten in large amounts. For example, a small portion of certain fruits may be fine, but larger servings could trigger symptoms.
- Plan your meals – Create a weekly menu using low-FODMAP recipes to ensure a balanced and stress-free diet. Include snacks and easy-to-prepare options to stay consistent, even on busy days.
- Join online communities – Support groups can provide helpful tips, recipes, and moral support from others managing FODMAP intolerance. These networks make the journey less isolating and more manageable.
In addition to diet, the best supplements for gut health and digestion can support your digestive health. Endorsed by Dr. Holly Lucille ND, RN, Gut Support Formula contains carefully selected ingredients designed to promote gut comfort and function. L-Glutamine is an amino acid that helps maintain the integrity of the intestinal lining, supporting a healthy gut barrier. This is especially important for those sensitive to FODMAPs, as a well-functioning gut lining can reduce discomfort.
Additionally, Slippery Elm has long been recognized for its natural ability to soothe the digestive tract, helping to alleviate occasional irritation. Together, these ingredients work to complement a healthy diet, offering extra support and balance as you navigate your journey toward better digestive health.
Is There a Link Between FODMAPs Intolerance and Mental Health?
Research suggests a strong connection between gut health and mental well-being, often called the gut-brain axis. For people with FODMAP intolerance, digestive discomfort may go hand in hand with mood changes, anxiety, or overall mental health challenges. This connection happens because the gut and brain communicate through the nervous system, hormones, and immune signals.
A 2021 study found that a low-FODMAP diet can influence gut bacteria. An imbalance in gut bacteria, often linked to FODMAP-related symptoms, may contribute to increased feelings of anxiety or emotional stress. Additionally, the fermentation of FODMAPs in the gut produces byproducts that could impact brain function and mood.
Although scientists are still exploring these links, keeping your gut healthy is an important part of supporting mental well-being. Following a low-FODMAP diet may help reduce physical symptoms while also creating a healthier gut environment. Over time, this could have a positive effect on mental health. If you notice mood changes alongside digestive issues, speak with a healthcare provider to get tailored advice.
Conclusion
FODMAP intolerance can significantly affect your digestive comfort, but it is manageable with the right approach. Identifying triggers through a low-FODMAP diet and making thoughtful food choices can help you take control of your symptoms. Replacing high-FODMAP foods with low-FODMAP alternatives, reading labels carefully, and planning balanced meals are essential steps in this process.
Remember, managing FODMAP intolerance isn’t about strict restriction – it’s about understanding what works for your body and creating a diet that supports your overall well-being. With proper adjustments and support, you can enjoy meals and maintain a healthy, comfortable lifestyle.
Yes, FODMAP intolerance can develop in adulthood. Changes in gut health, diet, or stress levels may affect how the body processes FODMAPs, leading to symptoms later in life.
FODMAP intolerance often overlaps with other food sensitivities, like lactose or gluten. While not directly related, similar digestive symptoms can occur, making it important to identify specific triggers through careful dietary observation or elimination diets.
Moderate exercise can support gut health by improving digestion and reducing stress, which may alleviate some symptoms. However, intense activity might worsen symptoms for some individuals, so a balanced approach is best.
Research continues to explore treatments like probiotics and gut microbiome modulation. While no cure exists, these approaches show promise in managing symptoms and improving overall gut health alongside a low-FODMAP diet.
Sign up for our Healthy Living newsletter!
Advertisement. This site offers health, wellness, fitness and nutritional information and is designed for educational purposes only. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk.