Does Glucose Rise When Hungry?
Does glucose rise when hungry? Discover why fasting increases blood sugar levels and learn natural strategies to maintain balance.


Many people assume that feeling hungry automatically means their glucose levels have dropped. This common belief leads to the idea that an empty stomach equals low glucose readings. However, the reality is more complex than this simple assumption.
But does glucose rise when hungry? Surprisingly, some individuals experience elevated glucose levels during fasting periods, even when they haven’t eaten for hours. This counterintuitive response can leave people confused about what’s actually happening in their bodies.
This article will explore the mechanisms behind fasting glucose elevation and provide practical strategies to help you maintain balanced glucose levels throughout the day.
Why Glucose Can Rise When You’re Hungry

Yes, glucose levels can indeed rise during fasting periods due to your body’s natural survival mechanisms that activate when you haven’t eaten for hours.
When you haven’t eaten for several hours, your body assumes it needs to maintain adequate glucose levels for essential functions. Rather than allowing glucose to drop dangerously low, your liver begins releasing stored glucose into your bloodstream. This process is triggered by hormones like glucagon and cortisol, which signal your body to produce glucose from internal sources.
The Dawn Phenomenon
The dawn phenomenon represents one of the most common examples of fasting glucose elevation. During early morning hours, your body naturally releases cortisol and growth hormone to prepare you for the day ahead. These hormones prompt your liver to release glucose, often causing elevated readings between 4-8 AM, even after an overnight fast.
Stress and Glucose
Cortisol, your primary stress hormone, plays a significant role in glucose regulation. When stress levels rise – whether from physical, emotional, or metabolic demands – cortisol triggers glucose production. This explains why some people experience higher glucose readings during stressful periods, regardless of their eating patterns.
Glucose Regulation Challenges
Fasting hyperglycemia occurs when your body’s glucose regulation system becomes less efficient. In healthy individuals, the body typically maintains tight glucose control. However, when cellular responsiveness decreases, glucose can remain elevated even during fasting states. This condition differs from signs of fast metabolism, where glucose is quickly processed and utilized.
Key factors contributing to elevated fasting glucose include:
- Prolonged stress exposure
- Poor sleep quality
- Hormonal imbalances
- Age-related metabolic changes
- Genetic predisposition
Understanding these mechanisms helps explain why glucose and hunger don’t always correlate as expected.
How to Know If Your Fasting Glucose Is High
Recognizing elevated fasting glucose often starts with paying attention to your body’s signals. Common indicators include persistent thirst, unexplained fatigue, frequent urination, and paradoxical hunger despite not eating for hours.
Physical signs to monitor:
- Excessive thirst that doesn’t subside after drinking water
- Unusual fatigue, especially in the morning
- Frequent nighttime urination
- Persistent hunger during fasting periods
- Difficulty concentrating or mental fog
Regular glucose monitoring provides the most accurate picture of your fasting levels. Check your glucose first thing in the morning, before eating or drinking anything except water. Consistent readings above normal ranges may indicate your body’s glucose regulation needs attention.
Furthermore, glucose targets can vary significantly with age. For those wondering what is normal glucose for seniors, it’s important to understand that acceptable ranges often differ from younger adults. Generally, fasting glucose levels between 80-130 mg/dL are considered reasonable for older adults, while younger individuals typically aim for 70-100 mg/dL.
Track your readings over time rather than focusing on single measurements. Patterns matter more than isolated high readings, which can occur due to stress, poor sleep, or temporary factors.
Simple Strategies to Balance Your Glucose Levels
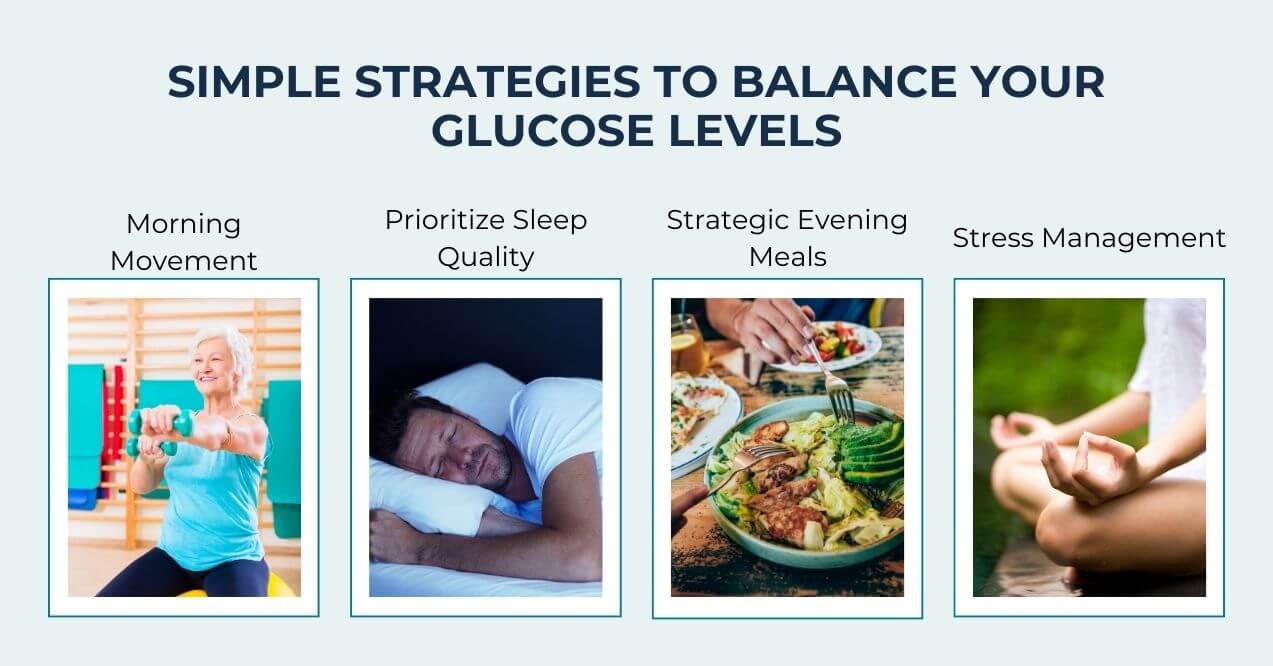
Managing fasting glucose requires consistent daily habits that support your body’s natural regulation mechanisms.
- Morning Movement – Start your day with physical activity to help regulate glucose levels. If you’re curious what exercises lower glucose the fastest, High-intensity interval training and resistance exercises show the most immediate impact, but even a 10-15 minute walk after waking can help reduce morning glucose spikes.
- Prioritize Sleep Quality – Maintain consistent sleep schedules to minimize the dawn phenomenon. Aim for 7-8 hours of quality sleep, going to bed and waking at the same time daily. Poor sleep disrupts hormone balance and can amplify morning glucose elevation.
- Strategic Evening Meals – Eat your final meal 3-4 hours before bedtime. Choose balanced dinners with adequate protein and fiber while limiting refined carbohydrates. This approach helps prevent overnight glucose surges that contribute to elevated morning readings.
- Stress Management – Practice daily stress-reduction techniques like deep breathing, meditation, or gentle yoga. Since cortisol directly influences glucose production, managing stress levels can significantly support healthy fasting glucose patterns.
While lifestyle strategies form the foundation of healthy glucose management, many people seek additional support for their fasting glucose concerns. Blood Sugar Formula offers a comprehensive approach with carefully selected botanicals and essential nutrients designed to support your body’s natural glucose regulation processes.

This comprehensive formula contains essential nutrients including Vitamin C, Vitamin D3, and Magnesium – ingredients that work synergistically to support your body’s natural glucose regulation processes.
For anyone seeking to naturally maintain healthy glucose levels and alleviate concerns about fasting glucose fluctuations, Blood Sugar Formula represents a new approach to daily glucose management and comfort.
Can Natural Alternatives Help Regulate Fasting Glucose?
Many individuals seek natural approaches to support their glucose regulation, particularly when experiencing fasting glucose fluctuations. Dietary supplements and herbal blends offer promising options for those looking to maintain healthy glucose levels through natural means.
Botanical Support Options – Various plant-based compounds have shown potential in supporting glucose balance. Cinnamon extract, chromium, and bitter melon are among the botanicals traditionally used to promote healthy glucose metabolism. These natural ingredients work by supporting your body’s existing glucose regulation pathways.
Nutritional Supplements – Essential vitamins and minerals play crucial roles in glucose metabolism. Magnesium supports cellular glucose utilization, while Vitamin D3 helps maintain proper glucose regulation. Vitamin C provides antioxidant support that may help protect glucose-regulating tissues.
Comprehensive Approaches – For those seeking a natural alternative to ozempic, combining multiple supportive nutrients often proves more effective than single ingredients. Well-formulated supplements that blend vitamins, minerals, and botanical extracts can provide comprehensive support for maintaining healthy fasting glucose levels.
Conclusion
So, does glucose rise when hungry? The answer is yes – fasting glucose elevation occurs due to natural hormonal cycles like the dawn phenomenon and metabolic imbalances that affect glucose regulation.
Understanding your body’s unique patterns is essential for maintaining optimal glucose balance. Start by tracking your fasting glucose readings to identify trends and triggers. Combine this monitoring with proven lifestyle strategies: regular exercise, consistent sleep schedules, balanced evening meals, and effective stress management.
Keep in mind that sustainable glucose balance comes from understanding your individual responses and implementing comprehensive approaches that work with your body’s natural processes rather than against them.
The dawn phenomenon causes this. Hormones like cortisol and growth hormone naturally rise during early morning hours, signaling your liver to release stored glucose into your bloodstream, creating elevated readings despite overnight fasting.
Results vary by individual. Some people benefit from intermittent fasting with improved glucose regulation. Others experience elevated fasting glucose due to metabolic challenges. Monitor your personal response patterns to determine what works best for you.
Yes, certain natural supplements may support healthy glucose levels. Products like Blood Sugar Formula contain vitamins and minerals that work with your body’s natural regulation processes to help maintain balanced glucose during fasting periods.
This combination may indicate your body’s glucose regulation system needs attention. Track these patterns consistently and consider consulting a healthcare professional to understand what’s happening with your metabolic processes and explore appropriate management strategies.
Sign up for our Healthy Living newsletter!
Advertisement. This site offers health, wellness, fitness and nutritional information and is designed for educational purposes only. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk.










