What’s the Connection Between Lymphedema and Cellulitis?
Master the basics of lymphedema and cellulitis care. Find practical lifestyle tips and early warning signs you shouldn't ignore.


Lymphedema and cellulitis often occur together, creating a cycle that can affect your daily life. When the body’s lymphatic system struggles to drain fluid properly, it leads to swelling that makes the skin more susceptible to infections. This article explores how these conditions interact, their early warning signs, and practical ways to maintain your well-being.
What’s the Connection Between Lymphedema and Cellulitis?
Your lymphatic system is your body’s drainage system. Lymphedema occurs when it’s damaged or blocked, causing fluid buildup and swelling, usually in the arms or legs, but sometimes in more uncommon places like preauricular lymph nodes. This can happen for a few reasons:
- Primary Lymphedema – Present from birth, due to problems with the lymphatic system.
- Secondary Lymphedema – Develops later due to surgery, cancer treatment, infections, etc.
While swelling usually affects limbs, it can sometimes appear near the ears, suggesting a lymphatic issue.
Now, let’s talk about cellulitis. It’s a bacterial skin infection (not to be confused with cellulite, the harmless skin dimpling). Cellulitis is serious, causing redness, swelling, pain, and warmth. Bacteria enter through cuts or breaks in the skin.
Here’s the connection: Lymphedema makes you much more likely to get cellulitis. The swelling stretches the skin, making it easier for bacteria to enter. And if you get cellulitis, it can worsen lymphedema by further damaging the lymphatic system. This creates a vicious cycle. Therefore, people with lymphedema must recognize cellulitis signs and seek immediate treatment.
Lymphedema and Cellulitis Warning Signs
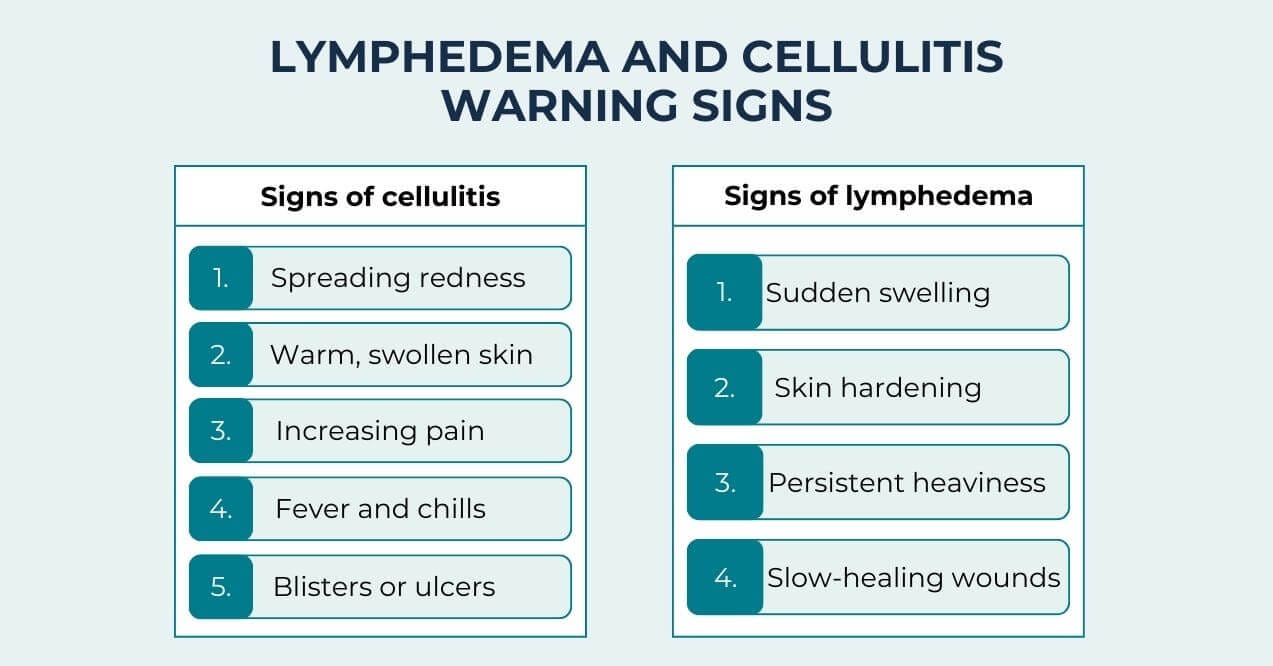
Identifying early warning signs helps prevent serious complications. Here are critical symptoms that warrant immediate attention:
Signs of Cellulitis
- Expanding areas of redness beyond the initial affected region
- Swollen, warm areas on the skin
- Increasing pain or tenderness
- Fever accompanied by chills
- Formation of blisters or skin ulcers
Worsening Lymphedema Symptoms That Require Attention
- Unexpected or severe swelling beyond regular patterns
- Changes in skin texture, including hardening
- Ongoing sensations of heaviness in affected areas
- Slow-healing wounds or persistent sores
Quick action when noticing these signs can help avoid more severe complications. Waiting too long may lead to extensive infections and lasting damage to your lymphatic system.
Lymphedema and Cellulitis Prevention and Management
Taking proactive steps helps minimize the impact of both conditions on your daily life. The connection between lymphedema cellulitis makes prevention particularly important, as managing one condition often supports the other.
- Proper skin care forms the foundation of prevention. Keep your skin clean and moisturized to maintain its protective barrier. When small cuts or scrapes occur, clean them promptly with mild soap and water, then cover with a fresh bandage.
- Many individuals with lymphatic concerns use compression garments to support circulation and comfort.. Properly fitted compression garments help maintain steady pressure on affected areas, supporting fluid movement through the lymphatic system. These garments work best when worn consistently during daily activities.
- Gentle movement supports both circulation and lymphatic drainage. Simple exercises like ankle rotations, arm circles, or hand squeezes can be incorporated into your daily routine. However, avoid strenuous activities that might stress affected areas.
- Regular skin checks help identify potential issues early. Take time each day to inspect your skin for any changes, particularly in areas affected by swelling. Good lighting and a mirror can help you examine hard-to-see spots.
Lymphedema and Cellulitis Lifestyle Tips
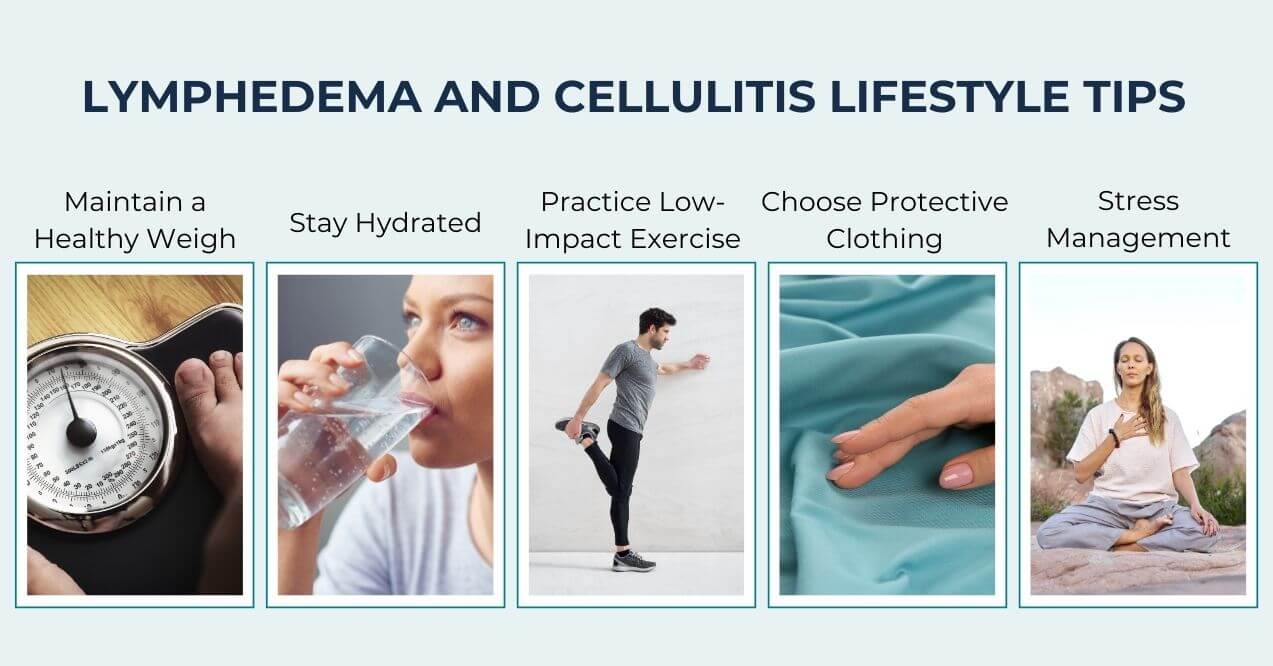
Your daily habits significantly influence how well you manage these conditions. Here are detailed approaches to support your overall well-being:
1. Maintain a Healthy Weigh
Extra weight puts additional pressure on your lymphatic system. Focus on fiber-rich foods like vegetables, fruits, and whole grains that provide sustained energy without excess calories. Include lean proteins such as fish, eggs, or legumes in your meals. Try eating smaller portions from a salad plate instead of a dinner plate. Take a 5-10 minute walk after meals to aid digestion and circulation. Small, sustainable changes often work better than dramatic shifts.
2. Stay Hydrated
Proper hydration supports your body’s natural processes. Start your day with a glass of water before breakfast. Set specific times for water breaks – with meals, between meals, and before bed. Enjoy hydrating foods like cucumbers, celery, and watermelon. If plain water becomes monotonous, add slices of lemon, lime, or orange for natural flavor. Track your intake with a marked water bottle or simple checkmarks on paper.
3. Practice Low-Impact Exercise
Begin with 5-10 minutes of seated ankle rotations and arm circles in the morning. Try water walking in a pool – the water’s natural pressure supports circulation while reducing strain on joints. Practice gentle chair yoga or stretching while watching TV. Aim for 2-3 short movement sessions throughout the day rather than one long session. Use a timer or link exercise to daily activities like commercial breaks or before meals.
4. Choose Protective Clothing
Select natural, breathable fabrics like cotton or bamboo that allow your skin to breathe. Look for clothing with flat seams to minimize skin irritation. Choose shoes with adequate toe room and soft insoles. Wear wide-brimmed hats and long-sleeved shirts with UPF protection during outdoor activities. In cooler weather, layer clothing instead of wearing one heavy garment. Check clothing regularly for signs of wear that might irritate skin.
5. Create Stress Management Routines
Start your day with 5 minutes of deep breathing or gentle stretching. Create a dedicated space for relaxation with comfortable seating and good lighting. Join a local gardening club or book group to combine social interaction with enjoyable activities. Listen to calming music or nature sounds during daily tasks. Practice simple mindfulness by focusing on the sensations of daily activities like washing dishes or folding laundry. Schedule regular times to connect with friends or family, even if just for short phone calls.
Final Thoughts
The relationship between lymphedema and cellulitis requires ongoing attention and care. By recognizing early warning signs and maintaining consistent self-care practices, you can better manage these conditions.
Take time to establish routines that work for your lifestyle. Small, daily actions add up to significant benefits over time. While managing these conditions takes effort, the right approaches can help you maintain your independence and quality of life.
Stay connected with healthcare providers who know your situation. They can offer specific guidance based on your needs and help adjust your management plan as needed. With proper care and attention, you can effectively manage both lymphedema and cellulitis while maintaining an active, fulfilling life.
Lymphedema makes the skin more susceptible to bacterial skin infections. The main concern is cellulitis, which causes redness, warmth, and swelling. The weakened skin barrier can also lead to fungal infections in affected areas.
Yes. Lymphedema stretches and weakens skin, making it more vulnerable to cellulitis infections. When cellulitis occurs, it can damage lymphatic vessels, which worsens lymphedema. This ongoing cycle continues unless proper management steps are taken.
During active cellulitis infection, lymphatic drainage should be avoided as it may spread the infection. However, once the infection clears, gentle lymphatic drainage helps reduce swelling and supports the body’s natural healing processes.
Sign up for our Healthy Living newsletter!
Advertisement. This site offers health, wellness, fitness and nutritional information and is designed for educational purposes only. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk.










